About Radion-D
Our Vision
Mission: Making Breast Radiotherapy Safer
Vision: To reduce dose to lungs and heart from breast cancer radiotherapy, and thereby the risk of radiation-related lung and cardiac morbidity and mortality, Radion-D promotes the prone crawl radiotherapy position using the Open Access Breast Couch (OABC). OABC expands the scope of prone radiotherapy to patients who require irradiation to the breast and regional lymph nodes. OABC is designed for techniques of prone deep-inspiration breath hold and state-of-art radiotherapy, including non-coplanar beam directions.
Our Story
Narrative behind breast cancer radiotherapy in prone crawl position

Introduction
By implementing intensity modulated techniques (IMRT) in the 1990s, we could improve breast cancer radiotherapy but not prevent high rates of acute toxicity, especially in woman with large pendulous breasts. As standard practice, patients were treated in supine position although other positioning techniques had been explored to decrease toxicity. The lateral decubitus technique developed at Institut Curie (Paris, France) in the 1950s and prone decubitus at Memorial Sloan-Kettering Cancer Center (New-York, USA) in the 1990s had demonstrated potential to decrease toxicity, with the largest benefits being documented for patients with large breasts.
At Ghent University Hospital, we were one of the pioneer centers worldwide to implement IMRT as standard practice. At the daily morning staff meetings in the department of radiotherapy, the research team documented the ability of IMRT to irradiate the breast using concave dose distributions that decreased collateral dose to heart and lungs, thereby lowering the long-term risks of radiation-induced cardiac and pulmonary side-effects. Prof. dr. Marc Mareel, radiation oncologist but mainly fundamental researcher on metastasis and invasion of cancer, attended the staff meetings. He never took vacation. He used a gentle form of the stick-and-carrot method. He missed no opportunity to make the point that our IMRT dose distributions were at-best a partial solution because he observed that many IMRT-treated patients still suffered from severe skin toxicity, mainly at the infra-mammary fold, and presented with fibrotic changes in the irradiated breast already during the first 2 years of follow-up.
2008-2013: change of practice from supine to prone (dive) breast radiotherapy
In 2008 we bought our first prone breast boards (Horizon, Civco Medical Solutions, Orange City, Iowa, USA) and started research on prone breast radiotherapy, thanks to support of the Foundation against Cancer and the National Cancer Plan. We modified the Horizon breast board to improve positioning and developed prone IMRT techniques for patients who needed whole breast irradiation (figure 1).
Mean age of our patients was above 60 years and despite the modifications only 70% of patients could be treated in prone position. Lack of comfort was the main problem with the Horizon breast board.
In 2009, we bought the AIO prone breast board (Orfit Industries, Wijnegem, Belgium) and modified it according to the experience gained with Horizon to obtain the roll of the patient’s body which is an important part of our IMRT technique (figure 2). With the more comfortable Orfit AIO more than 80% of patients could be treated in prone position.
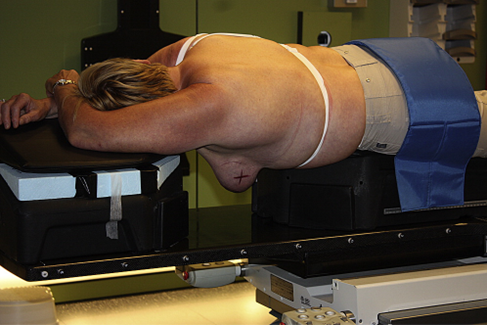
Figure 1: Patient treated on the modified Civco Horizon breast board. Image from Int J Radiat Oncol Biol Phys. 2012 Apr 1;82(5):2055-64.
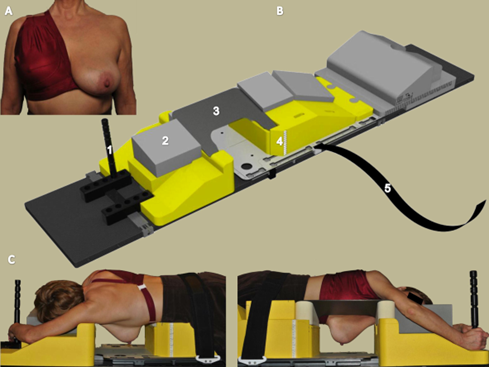
Figure 2: Patient positioning on Orfit AIO breast board. (A) Unilateral breast holder to retract the contra-lateral breast away from the treated breast. (B) Prone breast board: 1: hand grip; 2: head rest; 3: carbon fiber wedge support of the contra-lateral breast; 4: numeric scale (at both sides of the caudal part) to adjust table height using the in-room laser system; 5:
safety belt. (C) Ipsilateral (left panel) and contralateral (right panel) views of a patient positioned on the breast board. Image from Radiother Oncol. 2013 Aug;108(2):203-8.
By gravity the breast is pulled through the aperture of prone breast boards, away from lungs and heart (figure 3A). The increased distance between the irradiated breast, heart and lungs results in>70% dose reduction to the lungs and ~15% dose reduction to the heart. We were the first to perform prone breast radiotherapy during deep-inspiration breath hold (DIBH) which results in an additional 45% reduction of mean heart dose [1,2]. In prone position, the breast narrows in the direction of irradiation and skin folds are stretched.
These anatomical changes may explain the significantly reduced acute toxicity (figure 3B) and cosmetic changes (figure 3C) observed in a randomized trial comparing prone and supine radiotherapy [3,4]. These results caused a change of practice at Ghent University Hospital.
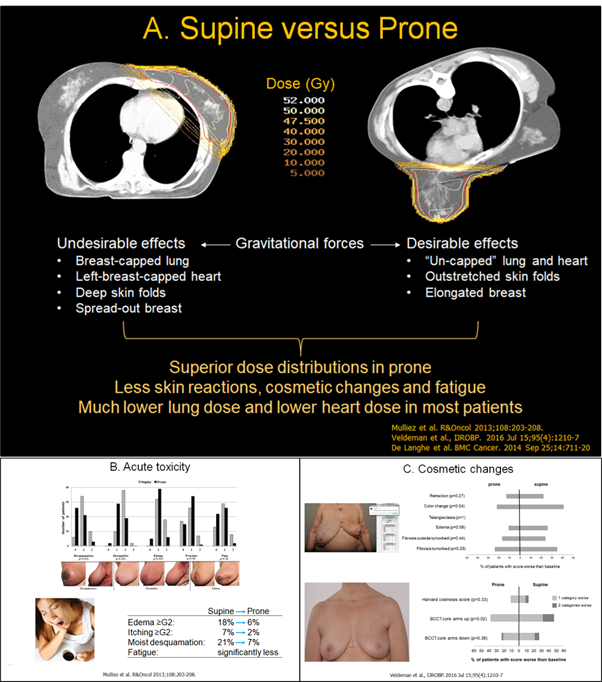
Figure 3: A. Gravity causes desirable anatomical changes for radiotherapy. Lower panels: results of a randomized controlled trial of supine versus prone breast-only radiotherapy in patients with cup size ≥C. A. acute toxicity and B. cosmetic changes.
From 2012 until 2019, AIO was our “work horse” prone breast board. Prone breast radiotherapy became treatment of choice for patients who required breast-only radiotherapy and who could reach and maintain the prone position on AIO.
2014-2019 development of the prone crawl radiotherapy technique
Treatment of regional lymph nodes is indicated in about 25% of the breast cancer patients who need post-operative radiotherapy. Adding the regional lymph nodes increases the irradiated volume which leads to more acute toxicity and higher risks of heart injury and lung cancer induction than in patients receiving breast-only radiotherapy. Before the last decade, only scarce attempts were made to treat the breast and regional lymph nodes in prone position. The main problem was lack of “open access” to the regional lymph nodes. The elevated arm at the side of the treated breast as well as parts of the breast board denied access of beams directions that target the lymph nodes while avoiding heart, lungs and contra-lateral breast. The need for a different patient position and a new design of the positioning system was obvious if we wanted to investigate prone breast and regional radiotherapy to decrease radiation toxicity in the most vulnerable patient population.
In 2012, we gathered information on different prone body positions that were used in medicine (surgery, intensive care) or sports (cycling, skeleton, swimming) hoping to get ideas towards a position with “open access” to regional lymph nodes. Crawl and skeleton positions came out as candidates for further investigations.
In 2013, a collaboration with the Industrial Design Center (High School West, Kortrijk, Belgium) started through the master thesis of Bert Boute MSc. PhD (figure 4).

Figure 4: Bert Boute photographed with Piz Lenin (7134 m, Kyrgyzstan) as background. After his PhD thesis defense, Bert started in 2019 his lifetime dream of traveling around the world by motorcycle (please continue reading the remaining of this narrative before watching “Interview with Bert Boute – The Story of B” or other video’s at Youtube).
At the final stage of Bert’s master thesis, the choice of the crawl position was made as direction for further research. During his PhD thesis (2014-2018), Bert became a key actor in the process of iterative co-creation involving breast cancer patients, radiation technologists, industrial designers, engineers, radiation physicists and oncologists. Prone crawl breast couch prototypes were designed, constructed, tested and redesigned. The aim of the UGent prone crawl project was stepwise elimination of the disadvantages of the prone positioning solutions that existed at that time (figure 5).
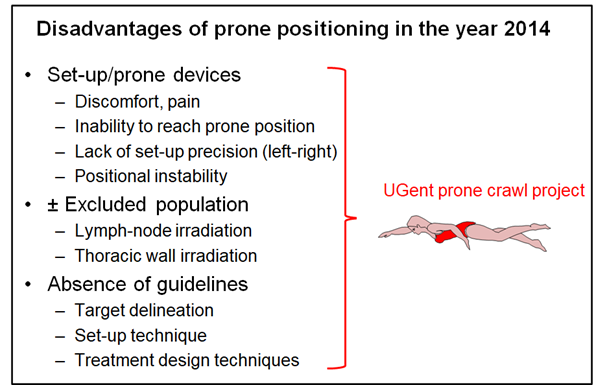
Figure 5: identification of challenges for using prone positioning in 2014.
Translational and clinical studies showed improved comfort [5,7], outstanding stability [6] and equal precision as supine positioning [7]. A preference survey showed systematic patient preference of
prone crawl position [7]. The strongest and distinguishing advantage of the Prone Crawl Breast Couch as compared to other prone breast devices is probably its performance in breast and regional lymph node irradiation including the internal mammary chain for photon- and proton therapy [8]. In this clinical setting, lung- and heart doses could be lowered to levels that have not been described with any other technique which translates to risk-reduction of radiation-related morbidity and mortality [8,9]. DIBH on the prone crawl breast couch proved to be robust [10] and can be prolonged to 3 minutes or more [11,12]. An MRI-compatible prone crawl breast couch was developed to acquire high-resolution imaging sets that were used to develop lymph node delineation guidelines [13].
2019-present: towards prone alone
Four operational versions of the prone crawl breast couch (coded PCBC1 to PCBC4) have been manufactured during the iterative co-creation process. PCBC1 and PCBC2 were involved in the translational and clinical studies that resulted in improved ergonomy. Regulatory requirements (EU Medical Device Directive) forced us to apply for CE-certification of PCBC3 because the primary endpoints of the studies were medical and not technological as was the case for PCBC1 and PCBC2.
Sixteen PCBC3 were manufactured to conduct multicentric studies (UH-Gent, Bordet Institute and UCL-CHU-Namur). The regulatory burden and the Covid-19 pandemic delayed the translational proces by almost 2 years. In 2020, PCBC3 became the workhorse for prone breast radiotherapy at UH-Gent. Using PCBC3 over 95% of breast cancer patients can be treated in prone position. PCBC3 has been implemented at Bordet Institute and UCL-CHU-Namur thanks to grants of the Foundation against Cancer and Think-Pink. During this Covid-19 pandemic, we developed PCBC4 and started EU’s new regulatory calvary (MDR since 2022) with the aim of medical and commercial valorisation of the patent “Radiotherapy Board and Couch” owned by Ghent University. The commercial name of PCBC4 is Open Access Breast Couch (OABC). Think-Pink will sponsor the cost of education and on-site training for all Belgian radiotherapy centers who switch from supine to prone breast radiotherapy in the period 2022-2023.
In the PhD-thesis of dr. Pieter Deseyne, radiation oncologist at UH-Gent, figure 6 can be found.
Currently, the citate in the legend of figure 6 applies to breast-only treatment which is indicated in 70-75% of breast cancer patients after breast-conserving surgery.

Figure 6: “In conclusion, compared to supine positioning, prone positioning has similar setup uncertainty, is not more time consuming, leads to lower OAR doses and has become significantly less uncomfortable for the patients. What are we still waiting for?” citate from the PhD thesis of dr. Deseyne.
The reluctance of main-stream radiotherapy in regard to a practice change from supine to prone treatment after breast conservative surgery is indeed intriguing. The lifespan of prone immobilization devices is such that hundreds -if not thousands- of patients can be treated after a single investment in the order of 10’s of thousands Euros with minimal device maintenance. Such investment in hardware and know-how is >10-fold less than investments which are currently made by numerous radiotherapy departments in SGRT, IGRT, MRI-linacs or proton therapy. These large investments are done despite the absence of high-level clinical evidence.
Our present clinical and translational research aims at gathering evidence behind the use of prone crawl radiotherapy for the setting of breast and regional lymphnode radiotherapy. Clinical evidence is necessary to supplement in-silico and pre-clinical evidence which allready exist [8-12]. I hope that we can expand the scope of “prone alone” to regional radiotherapy in the near future.
References
1. Mulliez T, Veldeman L, Speleers B, Mahjoubi K, Remouchamps V, Van Greveling A, Gilsoul M, Berwouts
D, Lievens Y, Van den Broecke R, De Neve W. Heart dose reduction by prone deep inspiration breath hold in left-sided breast irradiation. Radiother Oncol. 2015 Jan;114(1):79-84. doi:10.1016/j.radonc.2014.11.038. Epub 2014 Dec 9.
2. Mulliez T, Van de Velde J, Veldeman L, De Gersem W, Vercauteren T, Speleers B, Degen H, Wouters J, Van Hoof T, van Greveling A, Monten C, Berwouts D, De Neve W. Deep inspiration breath hold in the
prone position retracts the heart from the breast and internal mammary lymph node region. Radiother Oncol. 2015 Dec;117(3):473-6. doi: 10.1016/j.radonc.2015.09.030. Epub 2015 Oct 8
3. Mulliez T, Veldeman L, van Greveling A, Speleers B, Sadeghi S, Berwouts D, Decoster F, Vercauteren T, De Gersem W, Van den Broecke R, De Neve W. Hypofractionated whole breast irradiation for patients
with large breasts: a randomized trial comparing prone and supine positions. Radiother Oncol. 2013 Aug;108(2):203-8. doi: 10.1016/j.radonc.2013.08.040. Epub 2013 Sep 14
4. Veldeman L, Schiettecatte K, De Sutter C, Monten C, van Greveling A, Berkovic P, Mulliez T, De Neve W. The 2-Year Cosmetic Outcome of a Randomized Trial Comparing Prone and Supine Whole-Breast
Irradiation in Large-Breasted Women. Int J Radiat Oncol Biol Phys. 2016 Jul 15;95(4):1210-7. doi: 10.1016/j.ijrobp.2016.03.003. Epub 2016 Mar 10.
5. Boute B, De Neve W, Speleers B, Van Greveling A, Monten C, Van Hoof T, Van de Velde J, Paelinck L, De Gersem W, Vercauteren T, Detand J, Veldeman L. Potential benefits of crawl position for prone radiation therapy in breast cancer. J Appl Clin Med Phys. 2017 Jul;18(4):200-205. doi: 10.1002/acm2.12118. Epub 2017 Jun 26.
6. Boute B, Veldeman L, Speleers B, Van Greveling A, Van Hoof T, Van de Velde J, Vercauteren T, De Neve W, Detand J. The relation between patient discomfort and uncompensated forces of a patient support
device for breast and regional lymph node radiotherapy. Appl Ergon. 2018 Oct;72:48-57. doi: 10.1016/j.apergo.2018.05.002. Epub 2018 May 12.
7. Deseyne P, Speleers B, De Neve W; Boute B, Paelinck L, Vakaet V, Van Hulle H, Schoepen M, Stouthandel M, Monten C, MD, Van Greveling A, Post G, Depypere H, Veldeman L. Prone crawl positioning improves set-up accuracy and patient comfort in prone whole breast irradiation
(submitted).
8. Speleers BA, Belosi FM, De Gersem WR, Deseyne PR, Paelinck LM, Bolsi A, Lomax AJ, Boute BG, Van Greveling AE, Monten CM, Van de Velde JJ, Vercauteren TH, Veldeman L, Weber DC, De Neve WC. Comparison of supine or prone crawl photon or proton breast and regional lymph node radiation therapy including the internal mammary chain. Sci Rep. 2019 Mar 18;9(1):4755. doi: 10.1038/s41598-019-41283-1.
9. Speleers B, Schoepen M, Belosi F, Vakaet V, De Neve W, Deseyne P, Paelinck L, Vercauteren T, Parkes MJ, Lomax T, Van Greveling A, Bolsi A, Weber DC, Veldeman L, De Gersem W. Effects of deep inspiration breath hold on prone photon or proton irradiation of breast and regional lymph nodes. Sci Rep. 2021 Mar 16;11(1):6085. doi: 10.1038/s41598-021-85401-4.
10. Deseyne P, Speleers B, Paelinck L, De Gersem W, De Neve W, Schoepen M, Van Greveling A, Van Hulle H, Vakaet V, Post G, Monten C, Depypere H, Veldeman L. Reproducibility of repeated breathhold and
impact of breathhold failure in whole breast and regional nodal irradiation in prone crawl position. Sci Rep. 2022 Feb 3;12(1):1887. doi: 10.1038/s41598-022-05957-7.
11. Vakaet V, Van Hulle H, Schoepen M, Van Caelenberg E, Van Greveling A, Holvoet J, Monten C, De Baerdemaeker L, De Neve W, Coppens M, Veldeman L. Prolonging deep inspiration breath-hold time to 3 min during radiotherapy, a simple solution. Clin Transl Radiat Oncol. 2021 Feb 23;28:10-16.
12. Parkes MJ, De Neve W, Vakaet V, Heyes G, Jackson T, Delaney R, Kirby G, Green S, Kilby W, Cashmore J, Ghafoor Q, Clutton-Brock T. Safely achieving single prolonged breath-holds of > 5 minutes for
radiotherapy in the prone, front crawl position. Br J Radiol. 2021 Jun 1;94(1122):20210079.
13. Stouthandel MEJ, Kayser F, Vakaet V, Khoury R, Deseyne P, Monten C, Schoepen M, Remouchamps V, De Caluwé A, Janoray G, De Neve W, Mazy S, Veldeman L, Van Hoof T. Delineation guidelines for the
lymphatic target volumes in 'prone crawl' radiotherapy treatment position for breast cancer patients. Sci Rep. 2021 Nov 18;11(1):22529.
Our Team
 Wilfried De Neve - Founder and Chief Medical
Wilfried De Neve - Founder and Chief Medical
 Dina De Haeck - CEO
Dina De Haeck - CEO
 Patricia De Roover - Radiotherapeutic Technologist
Patricia De Roover - Radiotherapeutic Technologist
 Max Schoepen - Engineering and Design
Max Schoepen - Engineering and Design
 Annick Van Grevelingen - Training and Field Support
Annick Van Grevelingen - Training and Field Support
Responsibility
Patient Advocacy & Engagement
Patients are at the heart of everything we do. We listen and learn from patients, advocates, and caregivers to meet the evolving needs of patients everywhere.
Ethics & Compliance
At Radion-D, we act with integrity in all we do to fulfill our purpose, and our values guide us in making the right decisions ethically and responsibly so that our business can meet patient and societal needs. All our colleagues are expected to live our values and take ownership of compliance as we positively impact patients' lives and global health.
Merit-Based Diversity, Equity, and Inclusion
Everyone has something to offer. Diverse teams are more collaborative, more accepting of different perspectives, and more representative of the world we all share. Our culture of diversity, equity and inclusion is based on merit—one where hard work, talent, and contributions drive success, and barriers to opportunity are removed.
Environmental Sustainability
We recognize that environmental issues can result in profound societal and public health impacts. Our company purpose—Breakthroughs that change patients’ lives—guides our environmental sustainability priorities, with a focus on climate impact mitigation, conservation of resources, and the reduction of waste arising from our operations.
Privacy Principles
Personal data is at the core of scientific and medical innovation, and your personal health data can play a critical role in helping you and your care team manage your health and make informed health decisions. We understand the sensitivity of information about your health.
When you entrust us with your personal data, you can expect that we will act ethically and responsibly. In fact, we have established the following principles to help ensure your personal data is used appropriately and protected:
-
Respect.
We respect your privacy and your rights to make choices about the collection, use and sharing of your personal data.
Transparency.
We believe in being transparent about our use of personal data. We want you to understand what personal data we collect, why we collect that data and how that data may be used.
Appropriate Use.
We are thoughtful about the type and amount of personal data we collect and the ways we use your personal data to improve health and to advance breakthroughs that change patients’ lives. We believe in using data in ways that you would expect, consistent with our principles of Respect and Transparency.
Safeguards.
We believe that safeguarding data is essential to respecting privacy. We maintain technical and organizational controls designed to prevent the unauthorized access to or use of your personal data.
Partners





UGent: please read the about/history for a more detailed description of their contribution
Think-Pink: Think Pink has repeatedly supported us in the development phase. Current, they focus on prone breast radiotherapy for the benefit of the patient, and therefore fund the prone training to foster rapid implementation
Puzzle: Puzzle-Marketing believes strongly in the social benefits of OABC and decided to partner with us to create our website.
© 2026 Radion-D - Webdesign by Puzzle
