Scientific evidence behind the prone crawl radiotherapy technique
Reduction of breast cancer-specific mortality by radiotherapy after breast-conserving surgery is counter-acted by dose-dependent excess mortality mainly from radiation induced cardiac injury and lung cancer [1-4].
The absolute 15-year disease-specific mortality reduction by adjuvant radiotherapy was estimated to be 3.8% in patients receiving radiotherapy after breast-conserving surgery, the majority being node-negative [2]. Absolute 20-year disease-specific mortality was reduced ~8% after mastectomy and radiotherapy in node-positive patients [5]. Non-randomized evidence exists that disease-specific mortality reduction could be equal [6] or even larger [7, 8] if the internal mammary (IM) nodes are also treated. These data support the hypothesis that the survival benefit of adjuvant radiotherapy is greater in patients receiving irradiation of the regional lymph nodes. However, regional lymph node irradiation is known to increase heart and lung dose as compared to whole breast or chest wall alone treatment; the dose-increase being highest if also the IM-nodes are irradiated [4]. Long-term mortality from dose to heart and lungs may even annihilate disease-specific survival benefit of radiotherapy in patients with risk factors for lung cancer or cardiac disease [4].
Dose to lungs and heart can be decreased by treating patients in prone position instead of supine [9]. Prone positioning involves the use of a prone breast board or couch that consists of a support surface and a breast aperture. By gravity, the breast is pulled through the aperture, away from lungs and heart. The breast narrows in the direction of irradiation and skin folds are stretched. These anatomical changes may explain the significantly reduced acute toxicity and cosmetic changes observed in a randomized trial comparing prone and supine radiotherapy [10, 11].
Supine positioning remains standard in the majority of radiotherapy departments in spite of the evidence of superior dose distributions using prone breast radiotherapy. These disadvantages are related to many commercially available prone devices and to the scope of application. Device disadvantages include discomfort, positional instability and reduced precision. The scope of application is mainly whole or partial breast irradiation. Reports of prone irradiation of thoracic wall or regional lymph nodes are rare [12].
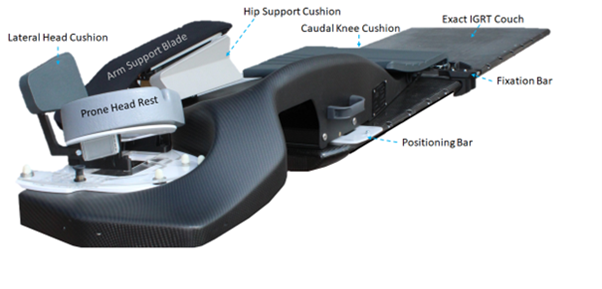
The OABC, developed by prof. dr. W. De Neve and his team at Ghent University, addresses many of the disadvantages of current commercial prone positioning devices. Its distinguishing feature is support in prone crawl position instead of the position with both arms elevated on commercial devices. Ergonomic and biomechanical studies resulted in highly improved patient comfort and stability [13, 14]. A comparative study showed that using a floor laser with the OABC resulted in equal set-up precision to standard supine treatment [15]. This study also showed that patient preference was the OABC instead of our commercial prone breast couch. In-silico trials, focusing on breast and regional lymph node irradiation, showed superior lung, heart, thyroid, esophagus and contralateral breast protection using the OABC as compared to the standard supine positioning device [16, 17].
Validated and innovative features of OABC
1/8: Improved stability of the patient
Non-ergonomic hard surfaces form the patient support side of most commercial prone breast radiotherapy devices. Soft mats or cushions are placed on the patient-support surfaces to make prone position bearable for the patient. Soft interfaces between patient and support surface lead to positional uncertainties and may reduce stability. Our goal was avoiding soft interfaces by designing ergonomic hard surfaces to support legs, pelvis, abdomen and contralateral hemi-thorax, shoulder and arm. Flat (non-ergonomic) surfaces that are typically used in commercial prone breast radiotherapy devices have the advantage of one-size-fits-all. The OABC features ergonomic patient support surfaces. To fit a vast range patient anatomies using ergonomic surfaces, we designed adjustable supports of head, ipsilateral shoulder and arm. Biomechanical studies were conducted to determine the design parameters of adjustable supports (degrees of freedom, range of motion) [13, 14].
2/8: More accurate positioning of the patient
A variety of tumor site-specific positioning devices that can be placed on and/or attached to the standard couches are commercially available in order to obtain a suitable position for radiotherapy. Standard radiotherapy treatment and CT-simulator couches have flat patient support surfaces. The OABC is designed as a positioning device to be placed on a flat surface. A design goal was vendor independence i.e. it should be possible to use the OABC with the standard CT-simulator or treatment couch of any vendor. All standard couches have lock points for positioning devices. Locking the OABC to the standard couch is done by the combination of a cranial standard transverse positioning bar and a caudal custom made clamping device that uses areas on the couches that are designed for locking of accessories. The positioning bar has 2 pins which dock in specific holes of the cranial anchorage component to secure unambiguous and accurate position of the OABC on the standard treatment couch. The clamping device also hosts a transverse bar with 2 pins which dock in specific holes of the caudal anchorage component providing redundancy on retaining the correct position. Hence, the OABC uses the table coordinate system provided by the vendor.
Most prone breast positioning devices have a basic symmetric design. Laterality is obtained by left or right side-specific add-on components which are mounted on the basic symmetric device part to treat left- or right-side breast cancer. The basic symmetric design imposes ergonomic restrictions. The standard prone position with both arms elevated (dive position) is roughly symmetric below the waist as well as cranial to the region of the patient’s breasts. The prone crawl position is asymmetric above the waist. Hence, the prone crawl position has more left-right asymmetry than the prone dive position. Early during the iterative process of prototype design-construction-evaluation, it became apparent that a basic symmetric design could not be united with good ergonomics. Therefore, we designed asymmetric left- and right-side prototypes in which striving for ergonomics was not anymore hampered by a need for symmetry.
Inaccuracies may increase by a tilted wedge used on many prone breast positioning devices which may also aggravate sinking of the patient. Furthermore, many patients have difficulties raising their arms above the head after surgery. The OABC addresses the problems mentioned here above. The claim of more accurate patient positioning is substantiated in reference 15.
3/8: Pain reduction
Patient positioning on commercially available devices leads to discomfort and pain making it impossible for >10% of the patients to reach the prone position or maintain it sufficiently long to execute a typical CT-simulation procedure or a treatment fraction. Regarding comfort, design objectives included a rate of ≤5% of patients who would be unable to receive prone radiotherapy for reasons of discomfort or pain. Pain reduction is substantiated in reference 15.
4/8: Facilitation of regional radiotherapy
In case of regional lymph nodal irradiation (LNI), commercially available prone breast positioning devices obstruct optimal beam paths by device parts that support the elevated arms of the patients. Their placement on top of the treatment couch makes sagittal positioning by laser lines on the breast and lymph nodes impossible. Therefore, laser lines on the patient’s back are used, which is suboptimal for left-right positioning of anteriorly located targets like the breast or axillary, peri-clavicular and internal mammary lymph node regions. The possibility to use a sagittal positioning laser on breast and the regional lymph node regions is shown in section “1.5 General description of the device”. Design objectives were keeping the medical advantages (less acute, mid-term and late toxicity) while avoiding the disadvantages (challenging and less precise patient positioning, position instability and poorly applicable for regional lymph node or thoracic wall radiotherapy) of commercially available prone breast radiotherapy devices. Potential of the OABC for regional radiotherapy is substantiated in references 13-17.
5/8: Dose- and risk reduction
Intensity-modulated radiotherapy and volumetric-modulated arc therapy made radiation more conformal. Image guided radiotherapy (IGRT) made treatments more accurate and precise, decreasing organs-at-risk (OAR) doses. OAR doses are further improved by breath hold techniques, a contralateral breast-holder, or changing the treatment position from supine to prone. The combination of these techniques yields the highest risk reductions of iatrogenic radiation effects. The OABC is unique regarding its performance in combining these techniques [18]. Radiotherapy for breast cancer implicates irradiation of surrounding OAR, which may cause side-effects like pneumonitis, fibrosis, ischemic heart disease, hypothyroidism, skin changes, and radiation-induced cancers. Reduction of OAR dose using the OABC leads to reduction of risk for developing radiotherapy-related morbidity and mortality which is substantiated in references 15-22.
6/8: Reduction of skin toxicity and aesthetic damages of the skin
In comparison to supine breast treatment, prone radiotherapy reduces skin toxicity and aesthetic damages [11]. This advantage is common to most prone breast positioning devices in the setting of whole breast irradiation. The distinguishing feature of the OABC is that it extends this advantage to the setting of breast and regional irradiation [preliminary data of the trial entitled “Whole breast (WB) and lymph node irradiation (LNI): prone compared to supine position in a randomized study with 15 or 5 fractions” AFMPS/SE/80M0671/. Clinical trial identification: Crawl-WB-LNI-1.0].
7/8: Designed for combining DIBH and prone patient positioning
The conclusion of a meta-analysis, comparing prone position versus supine position in post-operative radiotherapy for breast cancer, was that prone position combined with DIBH (P-DIBH) might become the most promising way for breast cancer patients to undergo radiotherapy [21]. Two new developments focus on the P-DIBH combination. First, a unilateral breast holder was developed in collaboration with Tricolast (Tricolast, Deinze, Belgium). The back-part of the breast holder is manufactured in skin-like tissue to facilitate surface-guided monitoring of the P-DIBH. Second, a transparent Head Support Component (HSC-TransView) is manufactured to allow visual feed-back for patients executing P-DIBH.
8/8: Efficiency in handling
Many prone breast radiotherapy devices consist of several components that are assembled ad-hoc on the CT-simulator or treatment couch. Other devices are directly positioned on CT-simulator or treatment couch as a single fully assembled unit. The design objective was a fully assembled unit for easy handling and efficient use.
References
1. Clarke, M., et al., Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet (London, England), 2005. 366(9503): p. 2087-106.
2. Early Breast Cancer Trialists' Collaborative, G., et al., Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10,801 women in 17 randomised trials. Lancet (London, England), 2011. 378(9804): p. 1707-16.
3. Berrington de Gonzalez, A., et al., Second solid cancers after radiotherapy for breast cancer in SEER cancer registries. British journal of cancer, 2010. 102(1): p. 220-6.
4. Taylor, C., et al., Estimating the Risks of Breast Cancer Radiotherapy: Evidence From Modern Radiation Doses to the Lungs and Heart and From Previous Randomized Trials. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 2017. 35(15): p. 1641-1649.
5. EBCTCG, et al., Effect of radiotherapy after mastectomy and axillary surgery on 10-year recurrence and 20-year breast cancer mortality: meta-analysis of individual patient data for 8135 women in 22 randomised trials. Lancet (London, England), 2014. 383(9935): p. 2127-35.
6. Hennequin, C., et al., Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy. International journal of radiation oncology, biology, physics, 2013. 86(5): p. 860-6.
7. Thorsen, L.B., et al., DBCG-IMN: A Population-Based Cohort Study on the Effect of Internal Mammary Node Irradiation in Early Node-Positive Breast Cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology, 2016. 34(4): p. 314-20.
8. Poortmans, P.M., et al., Internal Mammary and Medial Supraclavicular Irradiation in Breast Cancer. The New England journal of medicine, 2015. 373(4): p. 317-27.
9. Formenti, S.C., et al., Prone vs supine positioning for breast cancer radiotherapy. JAMA, 2012. 308(9): p. 861-3.
10. Mulliez, T., et al., Whole breast radiotherapy in prone and supine position: is there a place for multi-beam IMRT? Radiation oncology (London, England), 2013. 8: p. 151.
11. Veldeman, L., et al., The 2-Year Cosmetic Outcome of a Randomized Trial Comparing Prone and Supine Whole-Breast Irradiation in Large-Breasted Women. International journal of radiation oncology, biology, physics, 2016. 95(4): p. 1210-7.
12. Shin, S.M., et al., Breast, chest wall, and nodal irradiation with prone set-up: Results of a hypofractionated trial with a median follow-up of 35 months. Practical radiation oncology, 2016. 6(4): p. e81-8.
13. Boute, B., et al., Potential benefits of crawl position for prone radiation therapy in breast cancer. Journal of applied clinical medical physics, 2017. 18(4): p. 200-205.
14. Boute, B., et al., The relation between patient discomfort and uncompensated forces of a patient support device for breast and regional lymph node radiotherapy. Applied ergonomics, 2018. 72: p. 48-57.
15. Deseyne, P. et al. Crawl positioning improves set-up precision and patient comfort in prone whole breast irradiation. Sci Rep. 2020 Oct 2;10(1):16376.
16. Deseyne, P., et al., Whole breast and regional nodal irradiation in prone versus supine position in left sided breast cancer. Radiat Oncol. 2017 May 26;12(1):89-
17. Speleers, B.A., et al., Comparison of supine or prone crawl photon or proton breast and regional lymph node radiation therapy including the internal mammary chain. Scientific reports, 2019. 9(1): p. 4755
18. Speleers, B., et al., Effects of deep inspiration breath hold on prone photon or proton irradiation of breast and regional lymph nodes. Sci Rep. 2021 Mar 16;11(1):6085.
19. Vakaet V., et al. Prolonging deep inspiration breath-hold time to 3 min during radiotherapy, a simple solution. Clin Transl Radiat Oncol. 2021 Feb 23;28:10-16
20. Parkes MJ, De Neve W, Vakaet V, Heyes G, Jackson T, Delaney R, Kirby G, Green S, Kilby W, Cashmore J, Ghafoor Q, Clutton-Brock T. Safely achieving single prolonged breath-holds of > 5 minutes for radiotherapy in the prone, front crawl position. Br J Radiol. 2021 Jun 1;94(1122):20210079
21. Lai J, Zhong F, Deng J, Hu S, Shen R, Luo H, Luo Y. Prone position versus supine position in postoperative radiotherapy for breast cancer: A meta-analysis. Medicine (Baltimore). 2021 May 21;100(20):e26000. doi: 10.1097/MD.0000000000026000.
22. Pignol JP, Hoekstra N, Wilke D, Dahn H, Nolan M, Vicini F. Estimation of Annual Secondary Lung Cancer Deaths Using Various Adjuvant Breast Radiotherapy Techniques for Early-Stage Cancers. Front Oncol. 2021 Aug 9;11:713328. doi: 10.3389/fonc.2021.713328.
